Second Challenge Winners and Finalists
CAPC is excited to announce the winners and finalists of the second round of The John A. Hartford Foundation Tipping Point Challenge. We encourage exploration to inspire future innovation. You can contact the project team leader of the winning submissions to learn more.
Gold Winners
Silver Winners
Bronze Winners
Finalists
We are pleased to announce the finalists of the second Tipping Point Challenge. The list below was originally named part of the Top 25, twelve of which went on to become winners.
-
Bluegrass Care Navigators
“Creating Access to Palliative Care Across Settings”
The US health care system is maladaptive in meeting the needs of patients with seriously illness. Moreover, there are limitations to the Medicare hospice benefit that limit the ability of this patient population to receive health care that is concordant with their goals, preferences, and values.
Recognizing the unmet needs of the people living with serious illness in our communities, Bluegrass Care Navigators (BCN) has assiduously worked to create access to specialist-level palliative care. Creating this access is dependent on community partnerships and taking on financial risk. The clinical model and financing of their specialist-level palliative care programs varies based on setting. While BCN’s partnerships with hospitals have been a model to replicate for other communities, newer initiatives focus on community-based palliative care. In the past three years, BCN has expanded their community-based palliative care program to include home-based palliative care, office-based palliative care, palliative care in nursing homes, and home-primary care.
-
Capital Caring Health
“Virtual Pediatric Multidisciplinary Rounds Enhance Regionwide Program Cohesion”
Pediatric patients under concurrent care move back and forth between hospital and home/community care. Maintaining seamless communication is essential but can be a challenge when multiple providers in multiple institutions are involved. Pediatric programs often have few patients when compared to adult hospice in any community. Additionally, community-based programs often cover large geographic regions with many satellite offices, making in-person interdisciplinary team (IDT) meetings difficult. Adult providers continue to be less familiar with pediatric concurrent care practices than dedicated pediatric providers.
Capital Caring Health set out to bring all pediatric RN case managers (RNCM) under one division, while simultaneously creating a strong partnership with the major tertiary children’s hospitals in their region. The team leveraged teleconferencing technology (Zoom) to allow RNCMs to present and discuss patients under the direction of pediatric specialists. This virtual rounding program incorporates representatives from each children’s hospital and RNCMs from each region, who report high satisfaction and program efficacy.
-
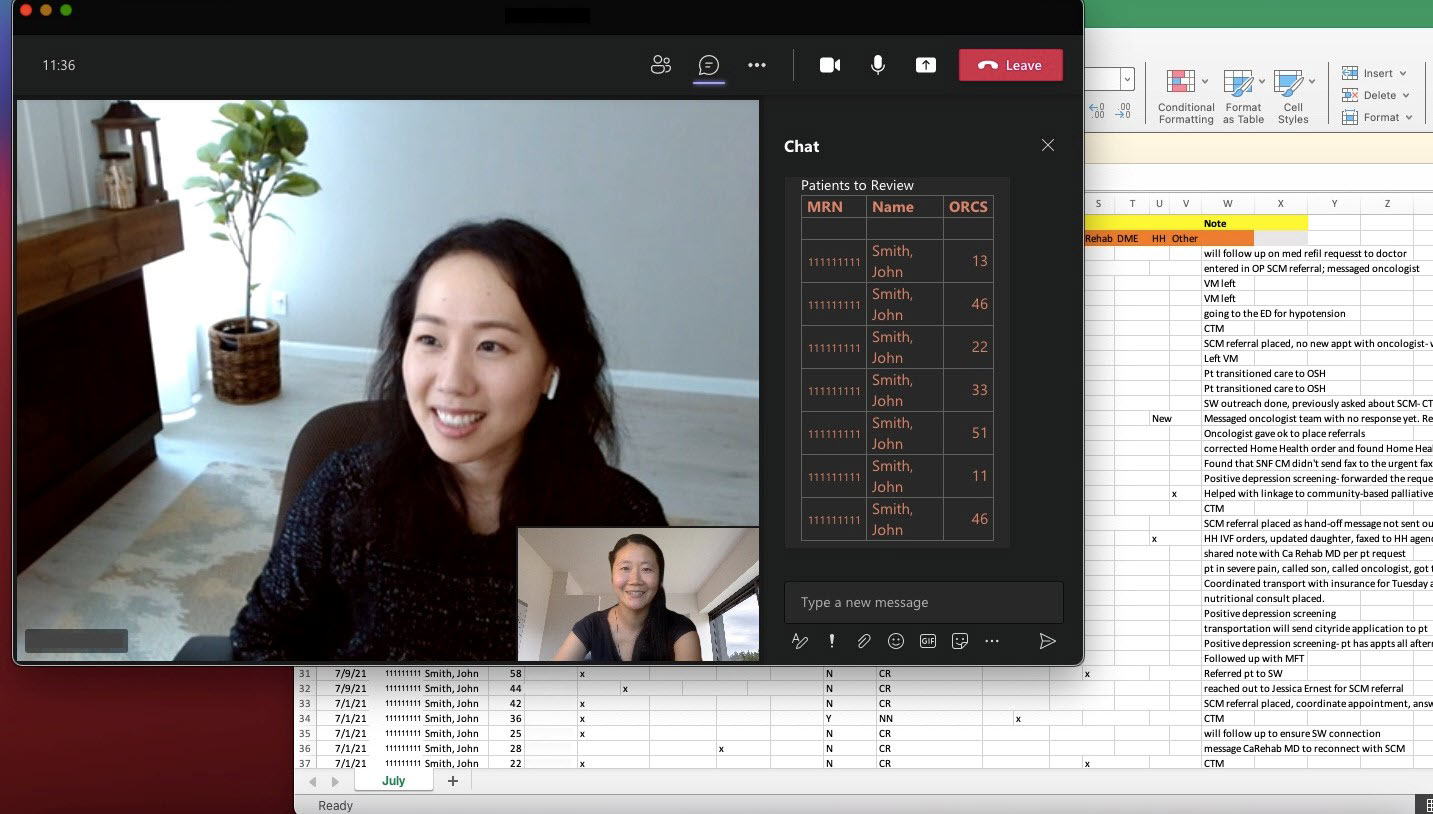
Cedars-Sinai
“Palliative Care for All: Improving Access Using a Population-Health Approach”
While Cedars-Sinai has sought to increase palliative care utilization among cancer patients, there remains significant room for improvement. This project aims to proactively identify patients with complex oncologic needs, provide linkage to palliative care, support patient care delivery, and improve health outcomes through the development of an Oncology Risk Composite Score (ORCS).
Upon implementation, the ORCS will monitor three different domains: 1) health care utilization; 2) patient-reported outcomes and screening; 3) and oncologic risk factors. Factors within each domain will be weighted to give both a domain and overall risk score, stratifying patients by risk level. A care coordination team will proactively reach out to identified patients and their care teams to implement necessary interventions, including palliative care consults, advance care planning, and other supportive care resources.
-
Commonwealth Care Alliance
“Promoting Primary Palliative Care Through Education and Standardized Documentation”
Commonwealth Care Alliance (CCA) is a health plan that provides care management and care delivery for dual eligible Medicare and Medicaid beneficiaries in Massachusetts. The organization recognized an opportunity to improve its approach to advance care planning (ACP) by improving education, training, and related documentation standards.
After CCA launched a chronic condition self-management program for CHF and COPD, which serves medically high-risk and behaviorally complex patients, they integrated ACP into the program. This solution has supported clinicians in addressing ACP, integrating members’ goals of care into their care plans. To do this, the team educated community-based advanced practice clinicians in communication skills to be able to conduct and document high quality ACP discussions.

-
Garnet Health Medical Center
“Mitigating the ‘July Effect'”
Each academic year, residency programs at Garnet Health Medical Center begin building a foundation of knowledge for their interns through boot camps, which focus on the “bread and butter” of the respective specialty. With management of patients living with serious illness often learned in the clinical setting, having this exposure is dependent on the intern’s schedule.
To help with this, Garnet Health Medical Center sought to educate internal medicine (IM) residents on palliative care competencies at the beginning of the academic year, introducing the care of seriously ill patients early on through a series of lectures. The team evaluated the impact of these lectures through questionnaires, assessing pre- and post- lecture trends. Through the assessment, they learned of a positive trend in the post-lecture questionnaires. The result: proposing the incorporation of palliative care education in lectures and simulations in intern boot camps throughout the year.

-
Institute for Human Caring, Providence St. Joseph Health
“Optimizing Palliative Care through Reducing Clinical Variation (RCV)”
After a call for initiatives by Providence St. Joseph Health to reduce unwanted clinical variation that challenge quality of care, efficiency, and costs, the Institute for Human Caring (IHC) responded with an innovative program. With the goal of improving palliative care clinical and program operations, they focused on three key objectives: increasing the percentage of PC referrals among non-OB adult inpatients (penetration); increasing the proportion of early inpatient PC consults; and decreasing the number of seriously ill inpatients with unmet need for PC. IHC built dashboards to track the metrics, while the palliative care team guided implementation.

-
Landmark Health
“Landmark: Illuminating a population health pathway to value-based Palliative Care”
Landmark Health is a risk-based, mobile medical group that cares for 140,000+ complex, chronically ill patients at home. It’s scalable palliative care focus proactively identifies those with serious illness, screens for needs and hospice eligibility and improves care through a holistic team-based approach.
All patients under their care receive and benefit from elements of palliative care. Their challenge: How do they take a population health approach to find which patients need heightened attention to goals of care and holistic management (symptom assessment, psychosocial/spiritual care)? How do they match them to the right intervention?
They approached this by: 1) reinforcing foundational palliative care skills and mindset for Landmark’s clinical team through training and local palliative physician leads and palliative social workers; 2) proactively identifying seriously ill patients before a crisis by combining predictive data analytics with clinician-driven assessments, and 3) leveraging technology-enabled operational and clinical workflows to manage patients in a consistent, scalable way.

-
Mercy
“Virtually Supported Complex Chronically Ill Patients”
In 2015, Mercy launched their virtual program, vEngagement, to improve care and reduce high costs from preventable ER and hospital utilization. Through the program, a multidisciplinary telemedicine team follows patients with complex chronic disease. Beginning in 2019, this team expanded their skillset to provide holistic care for people living with serious illness through the systematic incorporation of a palliative care approach to care. Training, workflows, and direct collaboration with a specialty palliative care physician empowered the virtual team to grow their symptom management and communication skills. As a result, all vEngagement patients now have access to advance care planning, serious illness conversations, and specialty palliative care consultation from the comfort of their homes, increasing the likelihood of goal-concordant care as chronic disease progresses.

-
Moffitt Cancer Center
“What Matters Most: NICHE-AFHS Interprofessional Project at Moffitt Cancer Center”
In pursuit of an Age Friendly Health System (AFHS), the Moffitt Cancer Center team chose to address “What Matters” to the cancer patient. In addition to asking and aligning care with each older adult’s specific health outcome goals and care preferences, they included end-of-life care preferences across the system, with question prompts that differed depending on the clinic and setting. For instance, in acute care settings, “What matters most today?” was asked every day on a whiteboard in patient rooms.
What started as low-tech paper made way for documentation in the electronic health record. The necessity for advanced directives and surrogate designation to be available to the health care team led to a design that provided a series of educational activities. This series empowered the nursing team to start the conversation and complete documentation of end of life preferences.
-
Porter Adventist Hospital (1)
“Impact of Early Palliative Care Consultation (EPCC) During the COVID-19 Pandemic”
Less than a month after the first COVID-19 Patient Under Investigation (PUI) was admitted to Porter Adventist Hospital, multiple rapid responses occurred on the COVID-19 medical floor requiring crucial ICU resources. Critical care and internal medicine physicians met briefly with palliative care (PC) Advance Practice Nurses (APRNs) to discuss the gap in early identification of goals of care. A collective decision was reached that every PUI would receive an automatic PC consult order.
The PC APRNs developed an innovative approach by requesting internal medicine hospitalists place PC consult orders upon admission while the PUI was still in the ED. Regardless of age, race, or co-morbidities, all PUIs were referred to PC, even though they may not have been referred to PC in another circumstance. EPCC resulted in more patients establishing decision-makers and goals of care prior to decompensation, thus helping patients avoid potential suffering caused by unwanted medical interventions.

-
Porter Adventist Hospital (2)
“Impact of a 2-Hour Intervention on Clinical Practice in End-of-Life”
Surveyed Americans report a preference to die at home; however, most die in institutional settings. Patients who are dying in the hospital have higher physical and emotional discomfort, lower quality of life, and prolonged grieving amongst caregivers; this population represents a vulnerable population requiring a specialized nursing skillset by acute care staff. Nurses report a lack of undergraduate training.
At Porter Adventist Hospital, an acute care hospital, a lack of knowledge and confidence was revealed in providing care to patients at end of life. To solve for this, the palliative care (PC) Advance Practice Nurses (APRNs) developed a 2-hour educational intervention for bedside nurses. After training, the nurses were able to demonstrate improved knowledge and self-efficacy. Research is underway to find the impact on clinical practice, with the hope to change nursing practice to improve the experience for the patient and family.

-
St. Tammany Health System
“Culture Shift Change within Rural South Louisiana Health System”
St. Tammany Health System (STHS) cares for a rural and suburban population; this includes Tangipahoa and Washington Parishes, which have respectively 24.9% and 21.7% of their populations living in poverty (per the U.S. Census Bureau). This compares to a statewide poverty average of 19.0% within Louisiana. These marginalized populations historically have had limited access to health care services.
STHS’ initiative aims to improve alignment of medical care received with the care desired by this marginalized, rural population. The goal is to improve integration of advanced care planning (ACP) services within the acute and post-acute settings for these communities. This included having the palliative care team broadening their scope to create a more comprehensive service, spearheading the standardization of ACP documentation.

-
Tufts Medical Center and Merrimack Valley Hospice
“Overcoming End of Life Disparities through Community Engagement and Education”
This innovative community outreach initiative between Tufts Medical Center palliative care and Merrimack Valley Hospice successfully engaged the Boston elderly Chinese American community conversation around serious illness, advance care planning, and end of life.
The palliative care team at Tufts started by identifying and addressing disparities in end of life care for traditionally underrepresented populations – through education specific to serious illness, such as cancer, end of life care and planning, and grief and bereavement. Through the early identification of the local Chinese-American immigrant community, the team fostered civic learning, completed a needs assessment, and educated and engaged the population in their health care.
This initiative enabled Chinese American community members and medical providers to engage in dialogue around sensitive/taboo topics, and represents a successful collaboration between a palliative care program and community-based non-profit organization serving elderly population in Boston’s Chinatown.














